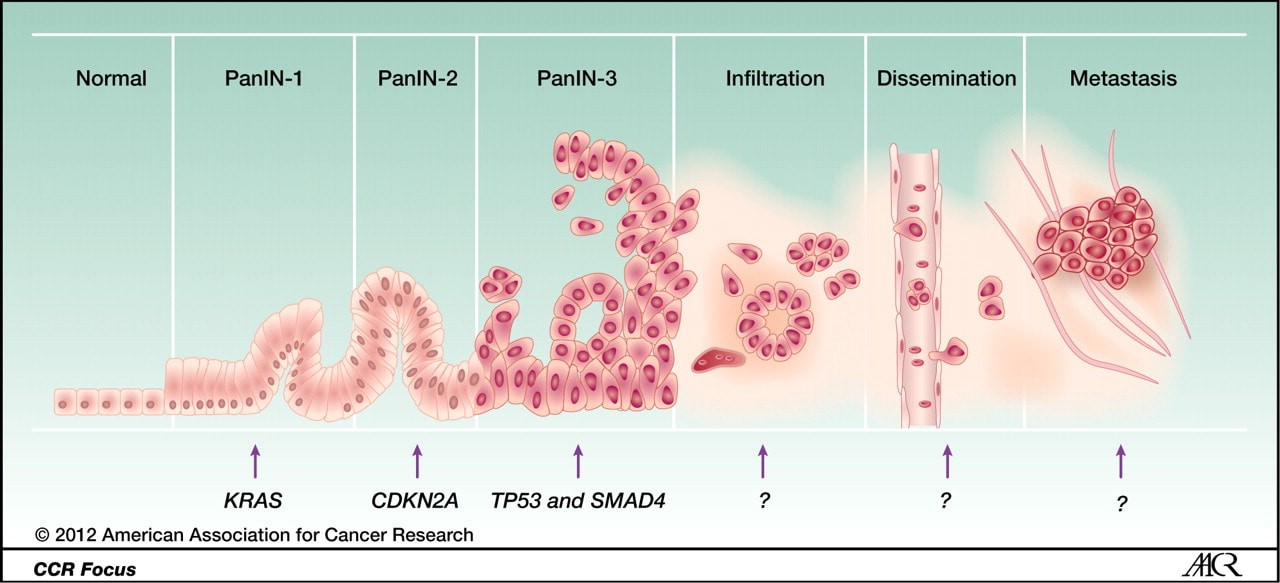
There are three different types of common pre-cancerous lesions known for pancreatic cancer. The first are "Pancreatic Intraepithelial Neoplasia" or PanINs. These are the small, non-fluid filled kind. There are different grades of PanINs, of increasing severity (PanIN 1 - PanIN 3). The lower grade PanIN 1 lesions are quite common in the population and most older people have at least a few. They are unlikely to ever cause any trouble. Conversely, PanIN 3 lesions are very rare, but also much more dangerous.
The other two types of pre-cancerous lesions are both larger fluid-filled types: Intraductal Papillary Mucinous Neoplasms, (IPMNs) are the more common of the two, and "Mucinous Cycstic Neoplasms". IPMNs vary in their location within the pancreas and their size, and these two features correlate with how dangerous they are. Luckily, IPMNs can be detected by imaging procedures, therefore making it possible to detect them before they become cancer. They are most often detected in patients who are routinely monitored due to a high familial risk, or incidentally in people who were imaged for another reason. If an IPMN is found in someone, a surgeon will have to make a determination as to whether it is a good idea to remove the lesion before it becomes actual cancer. This is a difficult decision to make because it involves balancing the risk of a patient developing cancer with the real risk of causing harm to the patient by removing a lesion that might never develop into cancer. This tough call is best made at a center that specializes in pancreatic cancer and sees a large number of pancreatic cancer patients.
"Mucinous Cystic Neoplasms" or MCNs are similar to IPMNs but, the principle difference between IPMNs and MCNs is how they look under a microscope, and how they behave in the patient (i.e. how likely they are to become cancer).
The other two types of pre-cancerous lesions are both larger fluid-filled types: Intraductal Papillary Mucinous Neoplasms, (IPMNs) are the more common of the two, and "Mucinous Cycstic Neoplasms". IPMNs vary in their location within the pancreas and their size, and these two features correlate with how dangerous they are. Luckily, IPMNs can be detected by imaging procedures, therefore making it possible to detect them before they become cancer. They are most often detected in patients who are routinely monitored due to a high familial risk, or incidentally in people who were imaged for another reason. If an IPMN is found in someone, a surgeon will have to make a determination as to whether it is a good idea to remove the lesion before it becomes actual cancer. This is a difficult decision to make because it involves balancing the risk of a patient developing cancer with the real risk of causing harm to the patient by removing a lesion that might never develop into cancer. This tough call is best made at a center that specializes in pancreatic cancer and sees a large number of pancreatic cancer patients.
"Mucinous Cystic Neoplasms" or MCNs are similar to IPMNs but, the principle difference between IPMNs and MCNs is how they look under a microscope, and how they behave in the patient (i.e. how likely they are to become cancer).