Pancreatic Ductal Adenocarcinoma
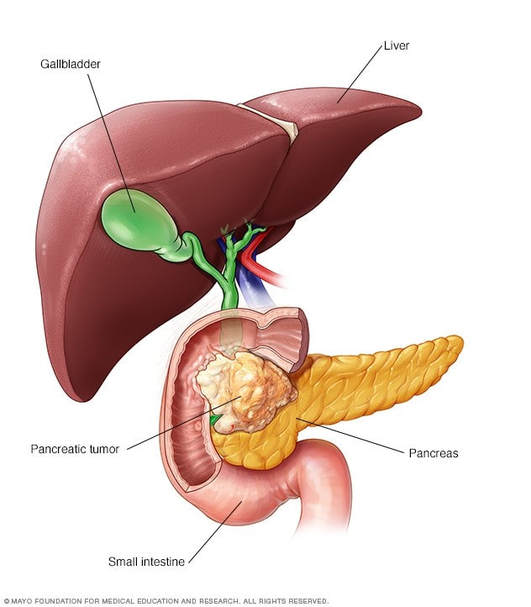
PDA is the most common malignancy of the pancreas. Pancreatic cancer is the 10th most common cancer in 2022 making up about 3.2% of all new cancer cases (1). PDA is an epithelial tumor, which is derived from the pancreatic ducts or ductules (2). A mutation in the Kras oncogene is the most common and earliest found PDA occurring in 90% of cases (2). Approximately 60-70% of PDAC arise from the head of the pancreas, whereas 20-25% arise from the body/tail (3).
Pancreatic cancer has the worst survival rate of any organ site, with a median survival of less than six months and a 5-year survival rate of just 11.5% (1). It is the fourth most common cause of cancer-related mortality, responsible for an estimated 49,830 deaths in the US in 2022 (1). Several factors contribute to this poor prognosis. Most patients (85%) present with advanced disease, precluding them from the one effective intervention: surgical resection. However, even among those with locally confined disease who have surgery, the 5-year and 10-year survival rates are just 25% and 8% respectively, due to high recurrence rates (3). For the remaining 85% of patients, as well as those with recurrent disease, there are few treatments available. The national standard-of-care therapy, gemcitabine, modestly extends survival by a few weeks, but was primarily approved on the basis of improved quality-of-life indicators (4). The only other FDA approved agent for advanced PDA is Tarceva, which provides an average of just 10 days additional benefit when combined with gemcitabine. Despite over 60 clinical trials of different agents and combinations,(5) no other effective therapies have been identified.
1. SEER Cancer Stat Facts: Pancreatic Cancer. National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/statfacts/html/pancreas.html
2. Stark, Alexander. Eibl, Guido. (2015). Pancreatic Ductal Adenocarcinoma. Pancreapedia: Exocrine Pancreas Knowledge Base, DOI: 10.3998/panc.2015.14
3. Modolell I, Guarner L, Malagelada JR. Vagaries of clinical presentation of pancreatic and biliary tract cancer. Ann Oncol 10 Suppl 4:82-84, 1999. PMID: 10436792.
3. H. Q. Xiong, K. Carr, J. L. Abbruzzese, Drugs 66, 1059 (2006).
4. A. Richter et al., World J Surg 27, 324 (Mar, 2003).
5. M. Tempero et al., J Clin Oncol 21, 3402 (Sep 15, 2003).
Pancreatic cancer has the worst survival rate of any organ site, with a median survival of less than six months and a 5-year survival rate of just 11.5% (1). It is the fourth most common cause of cancer-related mortality, responsible for an estimated 49,830 deaths in the US in 2022 (1). Several factors contribute to this poor prognosis. Most patients (85%) present with advanced disease, precluding them from the one effective intervention: surgical resection. However, even among those with locally confined disease who have surgery, the 5-year and 10-year survival rates are just 25% and 8% respectively, due to high recurrence rates (3). For the remaining 85% of patients, as well as those with recurrent disease, there are few treatments available. The national standard-of-care therapy, gemcitabine, modestly extends survival by a few weeks, but was primarily approved on the basis of improved quality-of-life indicators (4). The only other FDA approved agent for advanced PDA is Tarceva, which provides an average of just 10 days additional benefit when combined with gemcitabine. Despite over 60 clinical trials of different agents and combinations,(5) no other effective therapies have been identified.
1. SEER Cancer Stat Facts: Pancreatic Cancer. National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/statfacts/html/pancreas.html
2. Stark, Alexander. Eibl, Guido. (2015). Pancreatic Ductal Adenocarcinoma. Pancreapedia: Exocrine Pancreas Knowledge Base, DOI: 10.3998/panc.2015.14
3. Modolell I, Guarner L, Malagelada JR. Vagaries of clinical presentation of pancreatic and biliary tract cancer. Ann Oncol 10 Suppl 4:82-84, 1999. PMID: 10436792.
3. H. Q. Xiong, K. Carr, J. L. Abbruzzese, Drugs 66, 1059 (2006).
4. A. Richter et al., World J Surg 27, 324 (Mar, 2003).
5. M. Tempero et al., J Clin Oncol 21, 3402 (Sep 15, 2003).